Abstract
Background
Patients with stroke symptoms but negative diffusion-weighted imaging (DWI) might have transient ischemic attacks (TIA) or stroke mimics. Brain DWI is important for the diagnosis of cerebral infarction but it is not available before thrombolysis for most patients to avoid treatment delay. This study aimed to evaluate the safety of IV thrombolysis in patients with a negative post-treatment DWI for cerebral infarction.
Methods
We conducted a retrospective study of 89 patients treated with IV recombinant tissue plasminogen activator (rt-PA) within 4.5 h after stroke symptom onset. The patients were identified in our acute stroke registry from January 2009 to September 2010. Information on patients’ demographics, clinical characteristics, neuroimaging, treatment complications, and outcomes was obtained and analyzed.
Results
Out of 89 patients, 23 patients (26%) had a negative DWI on follow-up stroke imaging. Fourteen patients had a TIA and nine patients had a stroke mimic, including Todd’s paralysis, complicated migraine, and somatoform disorder. We found significant differences between patients with a positive and a negative DWI in mean age (62 years vs. 52 years; P < 0.01) and median admission NIH stroke scale score (11 points versus 6 points; P < 0.001). Among patients with a positive DWI, four patients had a symptomatic intracerebral hemorrhage (ICH). No patients with a negative DWI had symptomatic or asymptomatic ICH.
Conclusions
Our results suggest that the administration of IV rt-PA within the first 4.5 h of symptom onset in patients with suspected ischemic stroke is safe even when post-treatment DWI does not demonstrate cerebral infarction.
Similar content being viewed by others
Introduction
The administration of IV recombinant tissue plasminogen activator (rt-PA) is now recommended for selected patients with ischemic stroke up to 4.5 h from stroke symptom onset [1]. Magnetic resonance imaging (MRI) including brain diffusion-weighted imaging (DWI) is important for the evaluation of ischemic changes in patients with acute stroke but it is not available before thrombolysis in most institutions to avoid treatment delays. Therefore, the decision to treat a patient with IV rt-PA for acute ischemic stroke is based on the patient’s clinicoradiologic findings obtained from a brief and pertinent history, a neurologic examination using the NIH stroke scale (NIHSS), and a negative head CT scan for intracranial hemorrhage in agreement with current national guidelines. This limited approach for stroke diagnosis to avoid delays in the initiation of thrombolysis may result in an erroneous diagnosis of stroke which in turn may be conducive to the administration of rt-PA to patients with a stroke mimic.
Patients with stroke symptoms and a negative DWI might have either a transient ischemic attack (TIA) or a stroke mimic. Adding to the complexity of this clinical scenario, the sensitivity of DWI for the diagnosis of acute ischemic stroke is not 100% and a false-negative result is not uncommon during the first 24 h of ischemic stroke [2, 3]. The most frequently recognized stroke mimics are seizures with Todd’s paralysis, complicated migraine, and somatoform disorders [4, 5].
There are previous reports about the safety of IV rt-PA in patients with a suspected acute ischemic stroke within the 3-h treatment window, in whom the final diagnosis was not an ischemic stroke [6–8]. In a recent study, Chernyshev et al. [6] reviewed 512 patients treated with IV rt-PA in the first 3 h of symptom onset. They found 106 patients (21%) in whom a cerebral infarction was not visualized on follow-up stroke imaging. None of these patients had symptomatic intracerebral hemorrhage (ICH).
We aimed to study the safety of the use of IV thrombolysis in the first 4.5 h of stroke symptom onset in patients with negative post-treatment stroke imaging for cerebral infarction.
Methods
We conducted a retrospective study of 89 patients treated with IV rt-PA within 4.5 h of stroke symptom onset. The patients presented to our JCAHO-certified primary stroke center (PSC) or to one of the three satellite hospitals in our stroke network. The patients were identified in our acute stroke registry from January 2009 to September 2010. Information on patients’ demographics, clinical characteristics, neuroimaging including CT and MRI, treatment and its complications, and outcomes was obtained and analyzed.
In terms of neuroimaging, all patients had a pre-thrombolysis head CT scan followed by post-thrombolysis multimodal brain MRI and head and neck magnetic resonance angiography (MRA) in 87 of 89 patients. The diagnosis of TIA or stroke mimic was made retrospectively and it was based on the patient’s clinical presentation, hospital course, and a negative post-thrombolysis DWI for cerebral infarction. MRI was contraindicated in two patients in whom the diagnosis of stroke was confirmed after repeating a head CT scan in 3 days.
For statistical analysis, we used the t-test, the Mann–Whitney U test, the Chi-square test, and the Fisher exact test. A P-value of <0.05 was considered statistically significant. The statistical analysis was performed using SPSS for Windows.
Results
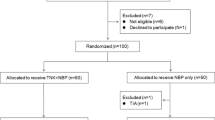
From January 2009 to September 2010, we treated 89 patients with IV rt-PA within 4.5 h of stroke symptom onset. One patient was excluded from our study because she passed away shortly after IV rt-PA infusion due to a ruptured aortic aneurysm. Twenty-three patients (26%) (six patients were treated within 3–4.5 h of stroke symptom onset) had a negative post-thrombolysis DWI for cerebral infarction completed within 24 h of admission. Of them, 14 patients (61%) had a TIA and nine patients had a stroke mimic: complicated migraine (n = 5), seizure with Todd’s paralysis (n = 3), and somatoform disorder (n = 1), as shown in Fig. 1.
Patients’ Baseline Characteristics
Table 1 provides information about of the patients’ characteristics at baseline. The patients with negative DWI were significantly younger (52 vs. 62 years old). With regards to other medical conditions, they had a significantly lower rate of arterial hypertension (57% vs. 80%) and a higher rate of psychiatric disease (17% vs. 3%). They also had a significantly lower NIHSS score (median 6 vs. 11 points) and a shorter hospital stay (5 vs. 9 days). There was no significant difference between patients with positive and negative DWI in terms of gender, history of diabetes mellitus, tobacco use, alcohol abuse, and previous history of ischemic stroke.
Patients’ Thrombolysis Information
Table 1 shows that more than a half of the patients who had a negative post-thrombolysis DWI received IV rt-PA in one of the three satellite hospitals of our stroke network as compared to our PSC (57% vs. 30%). This difference was significant. In the satellite hospitals, the decision to give IV rt-PA was based on a telephone consultation provided by the vascular neurologist on call for the brain attack team at the PSC to the emergency medicine physician attending the patient at one of the satellite hospitals. After the decision for thrombolysis was reached, IV rt-PA was given at the satellite hospital (“drip”), and the patient was then transferred to the PSC (“ship”).
Patients’ Safety Outcomes
Table 1 demonstrates that six patients (26%) in the DWI-negative group and 17 patients (26%) in the DWI-positive group received IV rt-PA within 3–4.5 h of stroke symptom onset. Among the patients who had a confirmed diagnosis of ischemic stroke (positive DWI), four patients had a symptomatic ICH (only one patient received thrombolysis within 3–4.5 h of symptom onset). None of the patients with a negative DWI had a symptomatic or an asymptomatic ICH on follow-up stroke imaging. The only complication among the latter group was gingival bleeding in one patient.
Discussion
We found that 26% of patients who received IV rt-PA with a pre-thrombolysis diagnosis of ischemic stroke did not have a cerebral infarction on follow-up neuroimaging in this study. The frequency of misdiagnosis of ischemic stroke ranges from 3% to 21% in other studies [6, 7, 9–11]. Our higher frequency of misdiagnosis might be partially explained by the fact that 57% of our patients received IV rt-PA at one of our stroke network satellite hospitals where only an emergency medicine physician evaluated the patient directly. Previous studies have demonstrated that emergency medicine physicians have difficulties distinguishing between a stroke and a stroke mimic during the emergency evaluation of stroke [9, 12]. In our study, the frequency of stroke mimics was 10% (n = 9) (95% CI 4–16) and it was in agreement with other studies in which the frequency of stroke mimics ranged from 7% to 31% [7, 12, 13].
In the present study, the patients with a negative DWI for cerebral infarction in follow-up stroke imaging were younger, had a higher frequency of psychiatric disease, and had a lower NIHSS score. These results were consistent with prior studies that found similar results [6, 7, 10].
None of our patients in the negative DWI group treated within 4.5 h of symptom onset had either a symptomatic or an asymptomatic ICH. This finding correlates well with previous studies in patients that received IV thrombolysis in the first 3 h of onset of symptoms [6–8]. These studies as well as our study have demonstrated that the use of IV rt-PA is safe in patients with suspected stroke in whom the “stroke” symptoms were in retrospect caused by a TIA or a stroke mimic. This result suggests that delaying IV thrombolysis in order to rule out a TIA or a stroke mimic is not warranted in terms of safety (e.g., getting stroke imaging with multi-modal brain MRI and MRA before IV rt-PA administration).
Our study has two important limitations related to its selection bias because it was retrospective, and its small sample size (23 patients had a negative post-thrombolysis DWI).
In conclusion, our study suggests that the administration of IV rt-PA within 4.5 h of stroke symptom onset is safe in patients with suspected stroke even if post-thrombolysis stroke imaging does not demonstrate cerebral infarction.
References
Lees KR, Bluhmki E, von Kummer R, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375:1695–703.
Schellinger PD, Bryan RN, Caplan LR, et al. Evidence-based guideline: the role of diffusion and perfusion MRI for the diagnosis of acute ischemic stroke: report of the therapeutics and technology assessment subcommittee of the American Academy of Neurology. Neurology. 2010;75:177–85.
Oppenheim C, Stanescu R, Dormont D, et al. False-negative diffusion-weighted MR findings in acute ischemic stroke. Am J Neuroradiol. 2000;21:1434–40.
Huff JS. Stroke mimics and chameleons. Emerg Med Clin North Am. 2002;20:583–95.
Yew KS, Cheng E. Acute stroke diagnosis. Am Fam Physician. 2009;80:33–40.
Chernyshev OY, Martin-Schild S, Albright KC, et al. Safety of tPA in stroke mimics and neuroimaging-negative cerebral ischemia. Neurology. 2010;74:1340–5.
Winkler DT, Fluri F, Fuhr P, et al. Thrombolysis in stroke mimics: frequency, clinical characteristics, and outcome. Stroke. 2009;40:1522–5.
Uchino K, Massaro L, Hammer MD. Transient ischemic attack after tissue plasminogen activator: aborted stroke or unnecessary stroke therapy? Cerebrovasc Dis. 2010;29:57–61.
Caplan L, Mohr J, Kistler J, Koroshetz W. Should thrombolytic therapy be the first-line treatment for acute ischemic stroke? Thrombolysis—not a panacea for ischemic stroke. N Engl J Med. 1997;337:1309–10.
Scott PA, Silbergleit R. Misdiagnosis of stroke in tissue plasminogen activator-treated patients: characteristics and outcomes. Ann Emerg Med. 2003;42:611–8.
Vroomen P, Buddingh M, Luijckx G, et al. The incidence of stroke mimics among stroke department admissions in relation to age group. J Stroke Cerebrovasc Dis. 2008;17:418–22.
Hand P, Kwan J, Lindley R, Dennis M, Wardlaw J. Distinguishing between stroke and mimic at the bedside: the brain attack study. Stroke. 2006;37:769–75.
Hemmen TM, Meyer BC, McClean TL, Lyden PD. Identification of nonischemic stroke mimics among 411 code strokes at the University of California, San Diego, Stroke Center. J Stroke Cerebrovasc Dis. 2008;17:23–5.
Acknowledgment
The authors wish to express their gratitude to James Roberts, B.S., R.N. for data collection assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Giraldo, E.A., Khalid, A. & Zand, R. Safety of Intravenous Thrombolysis within 4.5 h of Symptom Onset in Patients with Negative Post-Treatment Stroke Imaging for Cerebral Infarction. Neurocrit Care 15, 76–79 (2011). https://doi.org/10.1007/s12028-011-9523-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-011-9523-x